#BreakTheBias: Ending the silence surrounding pelvic floor disorders
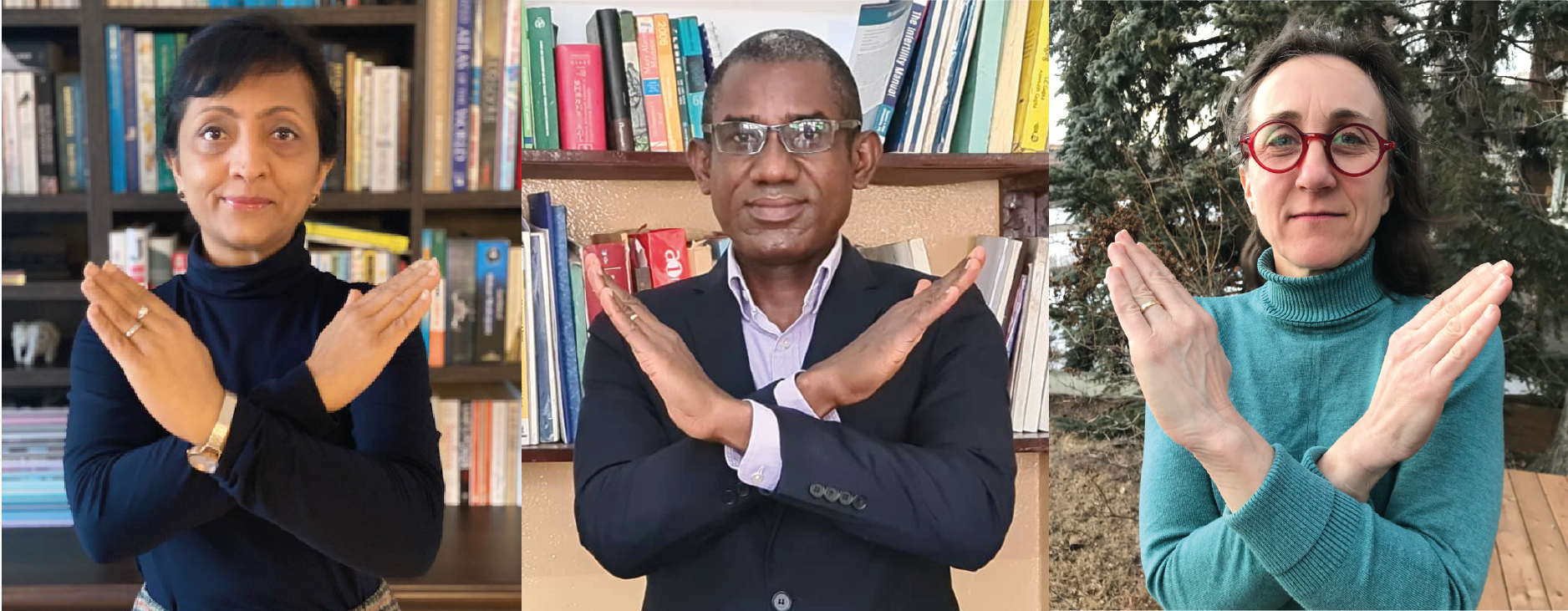
Ahead of this year’s International Women’s Day, with the theme #BreakTheBias, members of the Committee on Urogynaecology and Pelvic Floor Disorders discuss the stigma surrounding pelvic floor disorders. They highlight the importance of destigmatising these issues and educating health care workers to ensure that women can access the support that they need.

Urogynaecological or pelvic floor disorders (PFD) predominantly affect women following childbirth and the menopause. They are a wide range of conditions spanning the life spectrum. Notable among these are pelvic organ prolapse, urinary and faecal incontinence, pelvic trauma, sexual dysfunction and some malformations.
The FIGO Committee on Urogynaecology and Pelvic Floor Disorders articulates the issues related to pelvic health and bring the silent challenges faced by women and girls to the fore.
Bias and shame around pelvic floor disorders: the magnitude of the problem
Currently, many women do not seek help for urogynaecological or pelvic floor disorders. They suffer in silence and are reluctant to disclose these problems to a healthcare professional. The conditions they live with are heavily stigmatised – and because no one talks about what they are experiencing, everyone believes they are alone in facing these issues.
Prolapse and incontinence are an immense secret which affects women around the world. They are shrouded in shame, silence, isolation and lack of provision of care. In many instances, women living with a pelvic organ prolapse face social rejection and isolation due to their condition.
The impact of these conditions varies depending on the educational and socioeconomic status of women living with them. Often, women from disadvantaged backgrounds will accept these problems as an inevitability that cannot be addressed, due to the lack of available information.
Furthermore, women who are from more deprived nations are discriminated against in their access to treatment. For instance, in 2014, Amnesty International Nepal found that the government “failed to address the gender discrimination that underlies the causes of uterine prolapse thus failing to ensure Nepali women can exercise their sexual and reproductive rights.”
Raising awareness among healthcare workers
Even when women do seek treatment, caregivers can be dismissive of the problems they are facing, in spite of the existence of preventative measures and treatments available. These attitudes lead to further discrimination against women with PFD.
Raising awareness amongst healthcare providers to routinely ask about these problems is the first step to reducing bias in their management. Hence, there is a need for healthcare professionals to be educated about preventative measures. This will allow for women to be made aware of the need for pelvic floor muscle training during the antenatal period, and of the need to persevere with this habit throughout their lifetime.
FIGO’s role in promoting pelvic health
FIGO, through its Committee on Urogynaecology and Pelvic Floor Disorders, has pledged to increase awareness of these issues, not only amongst health care providers, but throughout the wider population and all stakeholders involved in women’s health care.
An education tool as simple as providing clinicians with screening questions (such as the ones highlighted below) will allow them to identify women suffering in silence and to offer adequate referral where necessary, hence promoting real change and providing support to thousands of women.
Example of screening questions for PFD
- Do you feel a bulge in the vagina or see something coming out of the vagina?
- Do you leak urine when you cough, sneeze, or laugh or when you rush to the bathroom and cannot make it on time?
- Is sex uncomfortable or painful?
- Do you have problems with stool control and leakage?
- If you answered yes to any of these, you do not have to live with this, request to see a urogynaecologist.