Guidance on the use of heat-stable carbetocin as an alternative to oxytocin in the prevention of postpartum haemorrhage
The International Federation of Gynecology and Obstetrics (FIGO) and the International Confederation of Midwives (ICM) issued a joint statement on the use of uterotonics to manage and reduce the complications of PPH in July 2021. That statement draws attention to a range of aspects of care that are essential to the prevention and treatment of PPH and recommends that all health care providers are trained and competent in both physiological and active management of the third stage of labour. This guidance builds on the 2021 joint statement and provides guidance on when heat-stable carbetocin should be considered as an alternative to oxytocin, and to caution against the inappropriate use of heat-stable carbetocin.
PPH is one of the leading causes of maternal mortality and morbidity globally, particularly among low- and middle-income countries and preventative measures are essential. FIGO and ICM are of the view that as policymakers, managers and clinicians operating in resource-constrained settings encourage the use of heat-stable carbetocin within countries, there might be an implication that oxytocin and heat-stable carbetocin indications are considered equivalent. They are not.
Uterotonics are recommended for use in active management of the third stage of labour. Oxytocin is supported as first-line uterotonic and needs continuous cold chain preservation to remain effective. Oxytocin is the recommended uterotonic for preventing and treating PPH, as well as for labour induction and augmentation. In contrast, heat-stable carbetocin is indicated only for PPH prevention. The inappropriate use of heat-stable carbetocin, similar to other existing uterotonics, can endanger the lives of women and babies. Education and monitoring, including pharmacovigilance, are paramount.
Carbetocin is a uterotonic recommended only for postpartum haemorrhage (PPH) prevention and should not be used:
- for labour induction or augmentation
- during pregnancy or labour (i.e. at any time before the baby is born)
- in women with cardiovascular disorders
- in women with liver or kidney disease
- in women with epilepsy
- in women with known sensitivity to heat-stable carbetocin, oxytocin or any of the excipients according to their composite (An excipient is an inactive substance that serves as the vehicle or medium for the active ingredients).
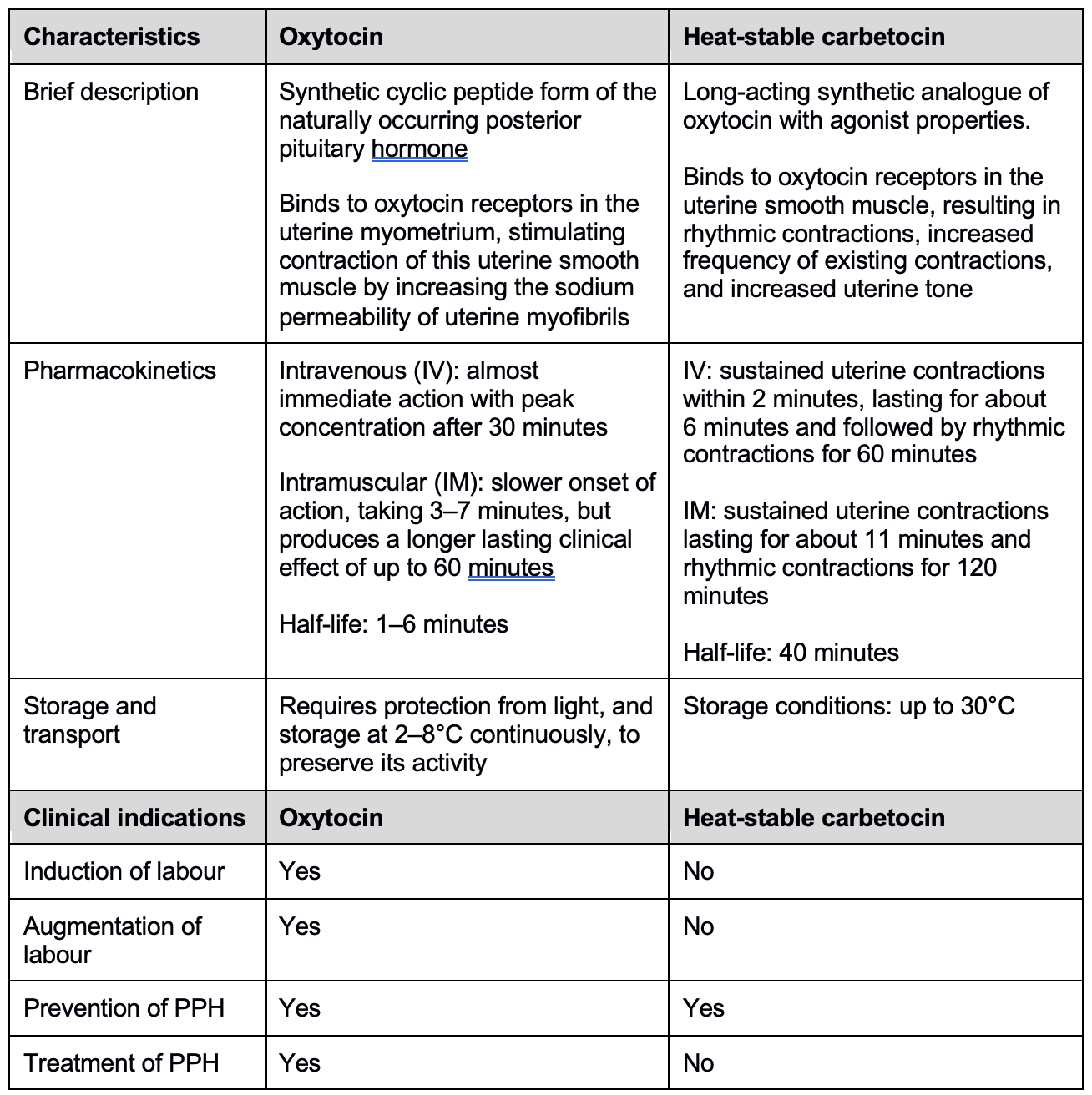
Heat-stable carbetocin – a uterotonic recommended only for PPH prevention – was added by the World Health Organization (WHO) to the core list of reproductive health medicines in the 2019 Model List of Essential Medicines. To remain stable and effective, all other injectable uterotonics (oxytocin, non-heat-stable formulation of carbetocin, injectable prostaglandins, and ergometrine) require cold transport and storage at 2–8°C. Heat-stable carbetocin overcomes the challenges of fragile cold chain infrastructure in struggling health systems. When used appropriately, heat-stable carbetocin plays a critical role in resource-challenged and warm-climate settings, where cold chain transport and storage is often not available and the quality of oxytocin and other injectable uterotonics is compromised. However, heat-stable carbetocin has different pharmacokinetic properties and is not considered to be an equivalent of oxytocin in terms of its pharmacological behaviours or clinical indications (see Table 1).
Table 1: Comparison of characteristics and clinical indications of oxytocin and heat-stable carbetocin (Source: WHO)
Low- and middle-income countries and those affected by fragility and humanitarian crises account for 94% of all maternal deaths globally. PPH currently accounts for approximately 25% of pregnancy-associated deaths worldwide and the majority of PPH deaths occur in women living in low-resource regions. PPH can be devastating for women and their families, with immeasurable effects on partners, children and communities. The severe maternal morbidities often associated with PPH are responsible for extended hospitalisations, additional procedures and prolonged recuperation. In most cases, maternal mortality can be prevented, and morbidity reduced, through prompt and evidence-based management by the perinatal team, including use of uterotonics, uterine massage, fluid replacement and tranexamic acid.
About our organisations
ICM and FIGO work together and with their extensive and globally diverse network of professional members to support women to achieve the highest standards of health and wellbeing, to keep birth normal and to promote equity for all women’s sexual, reproductive health and rights. ICM and FIGO promote the use of respectful, dignified and evidence-based care to reduce the global burden of maternal morbidity and mortality, of which the most significant contribution is postpartum haemorrhage (PPH), occurring during or within 24 hours of childbirth.
Quality care provided by midwives, obstetricians and gynaecologists contributes to the achievement of the Sustainable Development Goals (SDG) and the attainment of universal health coverage (UHC). FIGO and ICM develop standards and guidance for their respective professions that are aligned with World Health Organization (WHO) recommendations.
FIGO
FIGO is a professional organisation that brings together more than 130 obstetrical and gynaecological associations from all over the world. FIGO’s vision is that women of the world achieve the highest possible standards of physical, mental, reproductive and sexual health and wellbeing throughout their lives. We lead on global programme activities, with a particular focus on sub-Saharan Africa and South East Asia.
FIGO advocates on a global stage, especially in relation to the Sustainable Development Goals (SDGs) pertaining to reproductive, maternal, newborn, child and adolescent health and non-communicable diseases (SDG3). We also work to raise the status of women and enable their active participation to achieve their reproductive and sexual rights, including addressing female-genital mutilation (FGM) and gender-based violence (SDG5).
[email protected] | +44 (0) 20 7928 1166
ICM
The International Confederation of Midwives (ICM) supports, represents and works to strengthen professional associations of midwives throughout the world. The ICM has 143 members associations, representing 124 countries across every continent. ICM envisions a world where every childbearing woman has access to a midwife's care for herself and her newborn. ICM’s mission is to strengthen midwives' associations and advance the profession of midwifery.
ICM is an accredited non-governmental organisation representing midwives and midwifery to organisations worldwide to achieve common goals in the care of mothers and newborns. ICM works closely with the WHO, UNFPA and other UN Agencies; global professional health care organisations including FIGO, the International Pediatric Association (IPA), the International Council of Nurses (ICN), non-governmental organisations, and bilateral and civil society groups.
[email protected] | +31 (0) 70 306 0520
Referencing this statement
International Federation of Gynecology and Obstetrics, International Confederation of Midwives. Guidance on the use of heat-stable carbetocin as an alternative to oxytocin in the prevention of postpartum haemorrhage. 2023. Available from: www.figo.org/resources/figo-statements/guidance-use-heat-stable-carbetocin-alternative-oxytocin-prevention-postpartum-haemorrhage