Family Planning in high-income settings
Women in high-income countries need greater access to postpartum family planning. Dr Anita Makins, Project Director for FIGO’s Postpartum IUD project, explains.
Women in high-income countries need greater access to postpartum family planning. Dr Anita Makins, Project Director for FIGO’s Postpartum IUD project, explains:
As an OBGYN working on family planning counselling and provision across a range of resource settings, I firmly believe that postpartum contraception needs to be a greater priority in high-income countries.
There is a sense that, because women in higher-resource settings may achieve a greater level of education and awareness of their health needs, family planning services are automatically accessed. Data shows that this is not the case.
Ovulation can begin as early as 21 days post-delivery for women who are not exclusively breast-feeding – but recovering from labour, sleep-deprived, and busy with a newborn, the mother’s primary concern is generally not herself or her sexual health.
Up to one-third of full-term pregnancies in the UK are unplanned, and 1 in 13 women presenting for abortion or childbirth in a UK health board had conceived within a year of a previous childbirth.
Traditionally in the UK we address contraception at around six weeks post-delivery, which puts a lot of pressure on both the woman and the primary health care system. It is very clear that there is an unmet need for postpartum contraception, and we as OBGYNs are in a prime position to address this.
We first need to improve awareness of why appropriate birth spacing is so important. In higher-resource settings women are increasingly giving birth later on, with a tendency to squeeze in pregnancies. There is limited awareness of how short inter-pregnancy period is linked to maternal morbidity and mortality, as well as increasing your risk of preterm labour, miscarriage and infant death.
FIGO’s successful postpartum intrauterine device (IUD) project was established in six low-income settings, and it is vital for high-income setting providers to realise that expertise is not a one-way flow from north to south. There is a huge amount to learn from our colleagues around the world, and it was exciting to see the expansion of postpartum family planning in Scotland informed by our local partners working with the ministry of health in Sri Lanka.
During last year’s ICPD25 Summit in Nairobi I spoke at a session on identifying solutions for integrated sexual and reproductive health service delivery, and I think that is key. I have learned a lot from the way our partners in Bangladesh, India, Kenya, Nepal, Sri Lanka and Tanzania look at women’s health beyond protocols and specific clinical outcomes, and the idea that sexual and reproductive health does not only belong in a family planning clinic.
I think in high-income settings we have lost a little bit of that holistic perspective. Our training is so specialised that we can become very good at a particular niche element of women’s health, which does not necessarily help when considering the woman’s health needs as a whole.
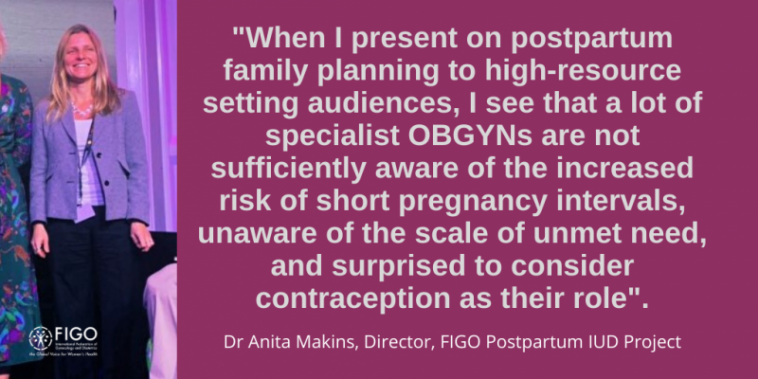
When I present on postpartum family planning to high-resource setting audiences, I see that a lot of specialist OBGYNs are not sufficiently aware of the increased risk of short pregnancy intervals, unaware of the scale of unmet need, and surprised to consider contraception as their role.
Every OBGYN should be able to counsel on family planning – providing balanced, non-coercive and quality care, where you give accurate information and take time to answer questions so that a woman can make an informed choice for herself and her family.
I am passionate about ensuring that women from all walks of life are able to live healthily and happily, and family planning is absolutely integral to women achieving their goals and desires.
As FIGO advocated throughout 2019, sexual and reproductive health and rights and gender equity are fundamental to the success of UHC. It was encouraging to see both of these priorities included in the United Nations Political Declaration of the High-Level Meeting on Universal Health Coverage, but now we need to hold our governments, and ourselves, accountable to these commitments.
For FIGO, this means working in close partnership with our 132 National Member Societies, and implementing projects that respond to their expertise and needs.
Cost remains a significant barrier to universal access to sexual and reproductive health-care. As OBGYNs we need to continue advocating for contraceptive services as part of UHC, with a method mix that is appropriate to each and every context. We are often asked why our postpartum IUD project is tied to a particular method, and the answer is that family planning needs to be sustainable. In many low- and middle-income countries, the copper IUD is the only consistently-available and affordable long-acting reversible contraceptive (LARC).
Contraception is part of a holistic package of healthcare, and a basic need for women to be able to lead happy, healthy lives. As OBGYNs, we are in a very great position to address it.