Self-Management of Abortion Project
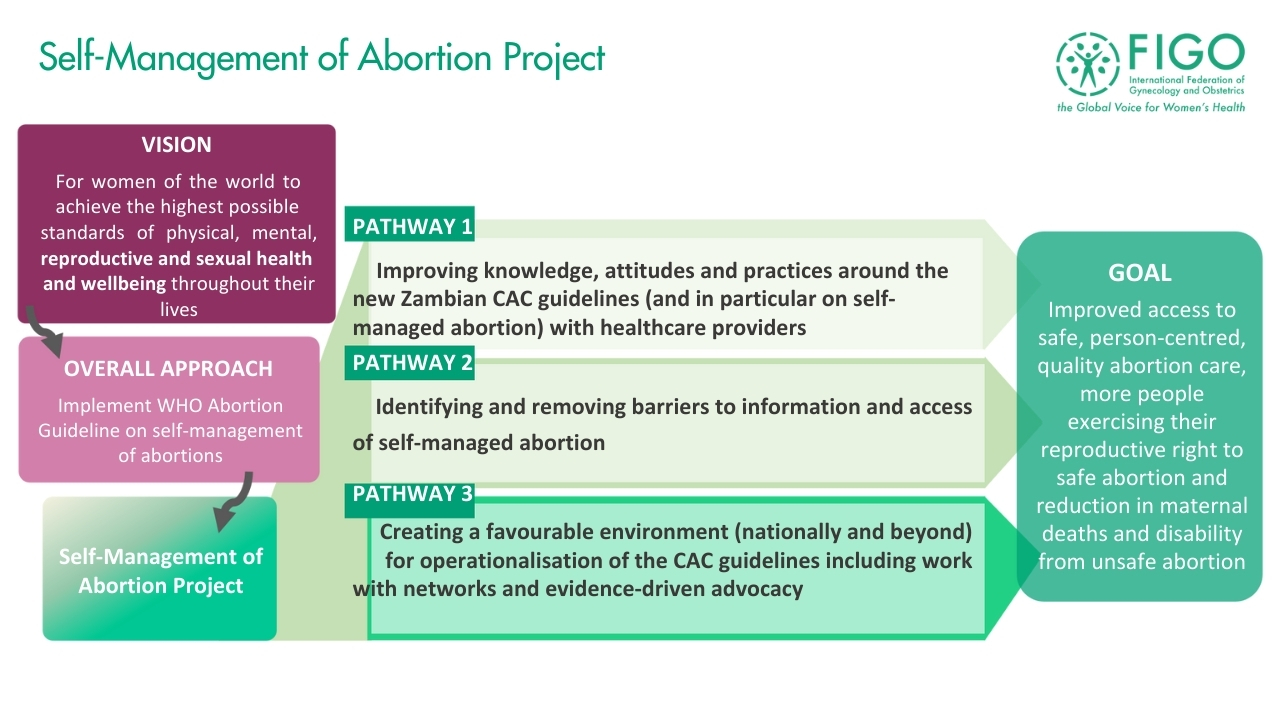
FIGO’s Self-Management of Abortion (SMA) Project, which concluded in May 2024, worked to implement WHO Abortion Guideline on SMA to improve access to safe, person-centred, quality abortion services.

Project contact
To contact the project team to ask a question about their work or to seek opportunities for collaboration, please click below.
Matthew Pretty, Project Manager
The importance of self-managed abortion
FIGO regards reproductive choice, including access to safe and quality abortion care, as a basic and non-negotiable tool for ensuring the human rights of every woman, girl and all people who can become pregnant not just in one region or country, but globally.
Improving access to safe abortion reduces preventable maternal deaths and disability. Finding ways to overcome the many barriers to access safe abortion is imperative, as is providing care in a way that meets the needs of women, girls and pregnant people.
Self-managed abortion is recommended in WHO Abortion Care Guideline 2022 and offers a strategy to overcome barriers including:
- Removing/reducing the time and cost to travel long distances to health facilities.
- Avoiding delays/inability to access care due to inadequate number of health facilities or staff able to provide abortion care.
- Reducing/avoiding barriers created by stigma by increasing privacy and autonomy.
How does self-management of medical abortion work?
In the first 12 weeks of pregnancy, a medical abortion can also be safely self-managed by the pregnant person outside of a health care facility (e.g., at home), in whole or in part. This requires that the woman, girl or other pregnant person has access to accurate information, quality medicines and support from a trained health worker (if they need or want it during the process).
Individuals clinically eligible for medical abortion may be offered the choice to self-administer a combination of mifepristone and misoprostol. The appropriate combination regimen consists of 200mg mifepristone, administered orally. This is followed 1–2 days later by 800μg misoprostol, administered vaginally, sublingually (under the tongue) or buccally (in the cheek). The minimum recommended interval between use of mifepristone and misoprostol is 24 hours. Mifepristone and misoprostol are available separately, or packaged together in the appropriate dosage. It can be taken anywhere, including at home. Direct supervision of a health-care provider is not required. Later, individuals can self-assess the completeness of the abortion process using pregnancy tests and checklists. Individuals should also have the option to immediately initiate contraception, should they desire it.
For more information see: WHO recommendations on self-care interventions.
What we do
FIGO is working with National Member Societies to support their work improving access to self-managed abortion. Initially, FIGO worked with the Zambia Association of Gynaecologists and Obstetricians (ZAGO) to operationalise the components of self-managed abortion in the new WHO comprehensive abortion care (CAC) guidelines to improve access to safe abortion services.
The project is identifying the barriers to implementation of self-managed abortion, and working to remove or reduce them, thus leading to improved access, financial and social benefits to patients, and reducing stigma around abortion care.
-Dr Swebby Macha, ZAGO President
The overall impact of this program was to reduce preventable maternal deaths and disability in Zambia from unsafe abortion. The Project team works closely with the FIGO Committee on Safe Abortion and international partners to promote the WHO Abortion Care Guideline (2022) and share best practice and lessons learnt.
Project details
This project ran for one year (June 2023 – May 2024) and was funded by CHAI. We worked through our member society Zambia Association of Gynaecologists & Obstetricians (ZAGO)
Project results
As a brief summary, improvements were seen in the knowledge of health care professionals, with the number trained to provide self-managed abortion increasing. There was increased understanding from providers of the benefits to women and girls, and healthcare facilities and providers, and increased confidence in women and girls’ ability to assess if their self-managed abortion was successful. Providers were shown to have changed their practice, with results showing an increase in those allowing women and girls to self-assess eligibility for SMA, and increased reference to guidelines, protocols and job aids on self-managed abortion.
In terms of the barriers to provision of self managed abortion in Zambia, on the provider side the project helped to improve drug availability; improve engagement from facility leadership; increase communication on self-managed abortions between HCPs and women and girls seeking care; and increase the provision of 2nd medication being taken at home. In the community, there were increased numbers of trained health community volunteers and improved acceptance of and preference for self-management of abortion by women and girls,
“The project has done very well to increase knowledge on SRHR, including safe abortion care. Also there used to be stock outs before the project started, but with the support from ZAGO, this has been addressed. We used to have problems with drugs and this project has really helped in this respect.”
-Pharmacist, Chipata DHO
Results from the project are summarised in this presentation and will be further outlined in two manuscripts which are under development.
Project resources
Recommendations and Best Practice for Self-Managed Abortion Projects
The project team produced this document summarising recommendations and best practices for other organisations or partners implementing self-managed abortion projects, based on the experiences from this project. The recommendations may need to be adapted based on the country context of the project being implemented.
Barrier Assessment Tool (BAT)
This tool was developed by the project team and used at baseline and endline evaluations to assess the barriers which might impede access to self-management of abortion. The tool covers different potential barriers at national, facility and community level, and was carried out with health care professionals at 30 facilities and members of their local communities. Whilst the tool was designed for the Zambian context, it could be adapted to other contexts.
Knowledge, Attitudes and Practices (KAP) Survey
This tool was developed by the project team and used at baseline and endline evaluations to assess the levels of knowledge, attitudes and practices of health care professionals in the target facilities with regards to self-management of abortion. The tool was carried out with health care professionals at 30 facilities. Whilst the tool was designed for the Zambian context, it could be adapted to other contexts.