New IJGO review provides comprehensive framework for preventing post-caesarean sepsis
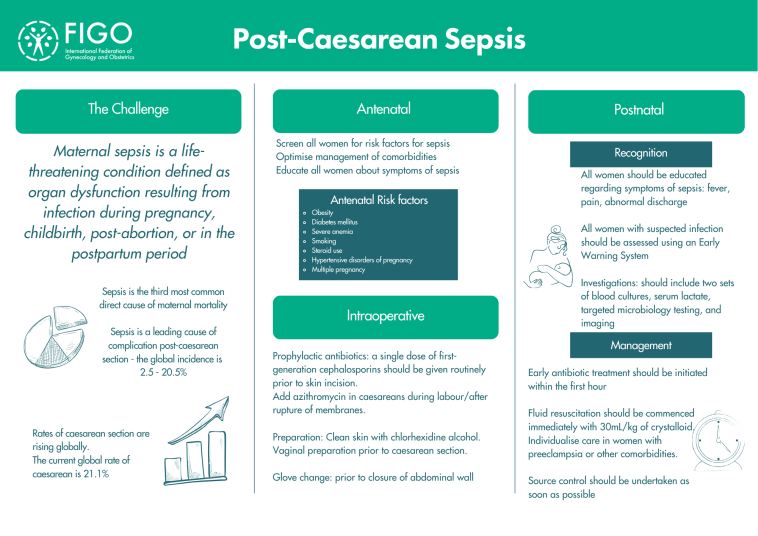
FIGO highlights critical new guidance published in the International Journal of Gynaecology and Obstetrics on preventing post-caesarean sepsis, a leading cause of maternal mortality.
The comprehensive review comes at a crucial time when sepsis accounts for 75,000 maternal deaths annually in low-income countries, with post-caesarean infection rates ranging from 2.5% to 20.5% globally.
Key prevention strategies
The paper emphasises that most cases of post-caesarean sepsis can be prevented through evidence-based measures. Prophylactic antibiotics administered 30-60 minutes before skin incision can reduce serious maternal sepsis by 70%. Vaginal antiseptic preparation significantly lowers postoperative endometritis rates, while skin preparation with chlorhexidine-alcohol has been shown to be more effective than iodine-based solutions. Safe surgical practices, such as changing gloves after placental delivery, also play a vital role in prevention.
The review also identifies important risk factors, including obesity (BMI >30), emergency caesarean delivery, prolonged labour and multiple vaginal examinations. Recognising these factors enables targeted strategies for women at higher risk of developing sepsis.
Caesarean section is lifesaving for mother and child when medically indicated. This paper provides clear, evidence-based guidance on preventing one of its most serious complications - post-caesarean sepsis - which occurs at a much higher rate than after vaginal delivery. This review outlines critical strategies, including appropriate preoperative antibiotic prophylaxis, proper skin and vaginal preparations, and glove changes prior to skin closure, to reduce infection risk. It also highlights the importance of early recognition and rapid management to save lives.
-Dr Edward Buga, corresponding author, member of the FIGO Committee on Infections During Pregnancy
Early recognition saves lives
Maternal sepsis must be treated as an obstetric emergency. With mortality increasing by 8% for every hour of delayed antibiotic treatment, the paper advocates for:
- implementation of pregnancy-specific early warning systems
- care bundles ensuring rapid assessment and treatment within one hour
- training healthcare teams in recognition and response protocols.
FIGO encourages all obstetric care providers to integrate these recommendations into practice and for healthcare systems to adapt protocols to local resources while maintaining core prevention principles.
The full review offers detailed guidelines for healthcare providers worldwide.